PERCEPTIONS and WONDERINGS
2024
Adagio
Albioni
The Organ and the Osteopath
In retrospect, playing three weddings three weeks after a laminectomy was not only foolish but most irresponsible of me; apparently the orthopedic surgeon had no idea of the stress on the torso and legs when playing a full pedal board on an organ. I wonder what would have happened if I had declined to play these three weddings so soon after the back surgery?
About ten years later under the care of the cranial Osteopath, I was so confident in this doctor, in this treatment that helped my body regain function that I once again became a classical church organist – for a very different reason. Postural strain induced on the back while playing a full pedal board mandates body positions that are unique to this instrument as well as the music that is being played.
Two legs dance around a full pedal board of thirty-two notes while two feet use both the heels and the toes. Two hands move between multiple manuals (keyboards) of varying heights, ten fingers strike the keys with different degrees of force, and there are numerous stops (voices) to the right and the left for altering sounds. At times, the hands can be playing high (to the right) and the feet playing low (to the left). This musical balancing act is most stressful for the entire body.
Playing the classical organ is the ultimate art of body balance and coordination to produce music.
Postural Demands
of the Classical Organ

My goal in returning
“to the bench”
was to reproduce these unusual
‘strained’ positions, to magnify those patterns embedded in the fascia*
after back surgery.
This amplification
of strain patterns assisted the
Osteopath in release and reduction
of pain and dysfunction.
- Fascia is a thin casing of connective tissue that surrounds and holds every organ, blood vessel, bone, nerve fiber and muscle in place.
- The tissue does more than provide internal structure; fascia has nerves that make it almost as sensitive as skin.

Initially, the headaches and backaches from playing two church services were extreme. I would go home and crawl into bed. My recurring Monday appointment after this ‘induced’ stress on Sunday gradually saw the headaches and backaches lessening. The changes and relief that transpired after these Sunday insults were astonishing… my confirmation and inspiration to continue this challenge to the ‘status quo’. I engaged in my organ playing rehabilitation activity for twelve months.
When the headaches and backaches weakened and my vitality and resilience increased despite the church services, I tearfully quit playing the classical organ. My piano graciously beckoned me and soothed my sorrow.
I reluctantly admitted that my organ activity was most stressful, literally ’embodied’, and could jeopardize my functionality in the long-term. Boxes of organ music sat on my closet shelf for thirty-five years before I was able to disengage one hundred percent. The music now lives on the shelves of a church that houses a magnificent pipe organ.
SBS
Spheno-Basilar Synchrondosis and Breech Birth
I wonder if the “abnormality” discovered at L5-S1 after the birth of my first child was a ‘congenital’ issue or ‘injury’ from the “saddle block” spinal anesthetic that left me paralyzed for four days?
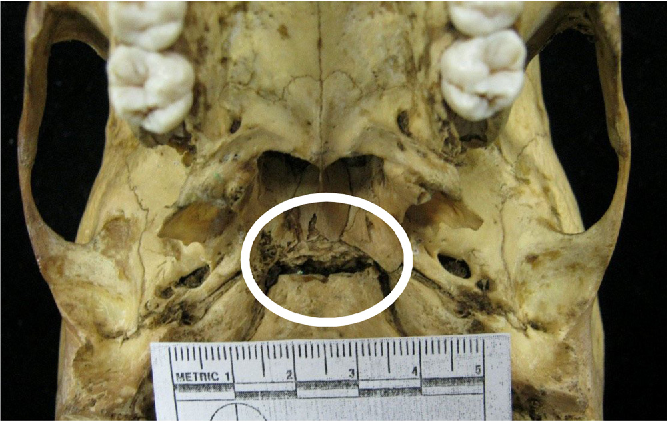
In the world of the cranial Osteopath, my breech birth could be the missing piece of information. The base of my skull (occipital bone) was and is an exemplary example of what breech delivery can do to the skull base, excellent for educational purposes with osteopaths-to-be in clinical rotation. In addition, breech delivery can easily misalign the spine because of the high probability of unequal force used when pulling the baby’s legs during delivery. In this instance, the osteopathic perspective provides relevant information that may or may not have been helpful after the first insult with anesthesia.
I also wonder how my own medical history would have been altered if I had received this kind of care at birth? I was a breech delivery, full term with low birth weight and placed in an incubator. I now know that cranial Osteopathic care of newborns can absolutely change the course of a life, especially in difficult deliveries and births. Based on my history of breech birth, there most likely was a ‘congenital abnormality’ in my low back as diagnosed by the orthopedic surgeon.
Today, my wondering has become quite sophisticated. Could the intubation trauma and PTSD experience in 1972 – four years before the back surgery – have triggered my autonomic nervous system into a chronic ‘hyper aroused, hypervigilant’ state? When coupled with a structural misalignment from my breech birth and the provocation from the ‘saddle-block’ anesthetic injection during the first childbirth, could this second birthing experience have predisposed my vertebrae for atypical motion three weeks after the laminectomy?
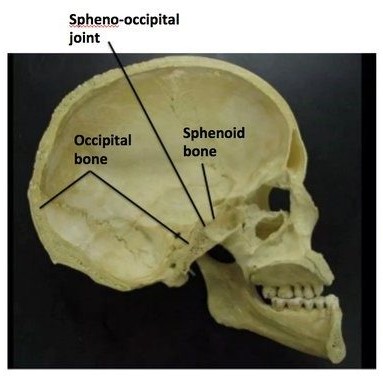
The base of the skull consists of the sphenoid base and the occipital base (Basi sphenoid, Basi occiput).
At birth, and several years following,
there is a joint that is movable. Forces applied during breech birth to the occiput are transmitted to this joint and can affect
the course of the person’s life.
The age of ossification (fusion) of this joint varies depending on growth spurts. This fusion process, beginning in the teens, is finished by age 25. In the cranial Osteopathic perspective, strain patterns between these two bones influence the stability and functionality of the autonomic nervous system. These strain patterns can be eliminated and/or reduced by the cranial Osteopath. The younger the child, the higher the probability of rapid positive change.
This junction, at the center of the skull, is called
the Sphenobasilar Synchrondosis (SBS) and/or
the Spheno-Occipital Junction (SOS).
Even after ossification, the skilled cranial Osteopath
is able to enhance the functionality –
biochemically, neurologically, emotionally
and structurally – of this central “Controller’,
located at the midpoint of the human skull.
Over the years, psychiatrists, otolaryngologists, neurologists, orthopods and dentists
as well as the cranial Osteopath have observed an
‘autonomic nervous system’ dysfunction.
I have always wondered if the initial trigger for these uncommon symptoms was the anesthetic trauma?
My body continues to confront and to release the remnants, residue and ramifications of this insult.
Fifty years later, I no longer wonder:
this injury in the throat (oropharynx) and insult to the autonomic nervous system,
a continuous vibration of ‘dissonance’,
not only undermined surgical attempts and recovery
but also complicated response to TMJ treatment.