PRIMARY RESPIRATORY MECHANISM
The Pressurestat Model

Semi-closed Hydraulic System

“A semi-closed hydraulic system is one in which there is a closed container with a regulated inflow and outflow mechanism. That is, fluid can be put into and removed from the container at controlled rates of flow. In this way, the quantity of fluid within the container at any given time can be regulated. If fluid is pumped into the container after it is full and at one atmosphere of pressure, and if the container cannot further expand its volume, the following conditions may occur: 1) the pressure inside of the container is increased until either the container springs a leak or explodes; 2) the pressure inside the container exceeds the pumping force which the inflow pump can produce; 3) the outflow system is opened to remove some fluid; or 4) the inflow pump is shut off. “
“This description fits the Pressurestat Model of the craniosacral system.”
(Upledger, Overview of Craniosacral Therapy, Upledger Institute International)
The mechanical reciprocal tension membrane system is only a partial representation of the craniosacral system. The dural membrane system houses the cerebrospinal fluid. It is the behavior of this fluid that completes an understanding of the craniosacral concept. The fluid within this ‘semi-closed hydraulic system” is known as the cerebrospinal fluid (CSF).
– Fluid enters the system via the choroid plexus which serves as a selective passageway for blood solutes from the vascular system into the ventricular system of the brain.
– The cerebrospinal fluid ls returned to the venous system by the arachnoid which are mostly concentrated in the superior sagittal sinus but are also found throughout the cranial venous drainage system.
The choroid plexus and arachnoid villae are under homeostatic control and serve as the regulatory mechanisms for the intake and outflow of this system. The shape of this hydraulic system is governed by fluid pressure within the dural membrane and by the cranial bones themselves which serve as anchors to which the membrane is firmly attached. The cranial bones are simply regarded as “hard places” in the dural membrane and are used as levers in treatment and as indicators in diagnosis.
(Figure 9) (Upledger, 1983)
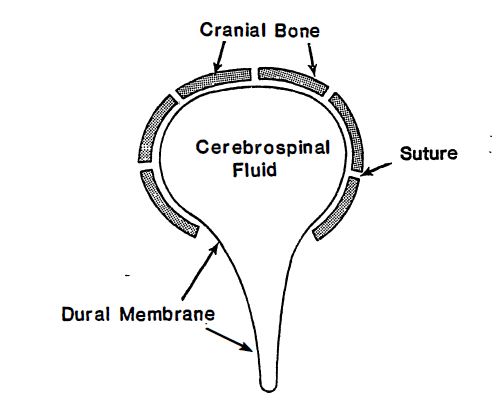
Dr. John Upledger (1983) has proposed a Pressurestat Model that offers an explanation of cranial motility. In this model, the cerebrospinal fluid production by the choroid plexus is more rapid that the resorption of the cerebrospinal fluid by the arachnoid bodies. When an upper threshold is attained, a homeostatic mechanism would stop production of cerebrospinal fluid. When the intracranial pressure causes the suture to open to a specific dimension, a stretch reflex is activated that signals the ventricular system to stop production of cerebrospinal fluid. When the suture begins to compress, the intracranial cerebrospinal fluid pressure is reduced. The brain is then signaled to produce more cerebrospinal fluid. (Upledger, 1983)
This relay system has been histologically confirmed by Dr. Ernest Retzlaff. Dr. Retzlaff has traced single nerve axons extending from the sagittal suture through the meningeal membranes to the wall of the third ventricle. (Retzlaff, 198)
Dr. Upledger thus conceives of a pressurestat mechanism acting upon the ventricular system of the brain. This pressurestat mechanism serves as the driving force of the inherent cranial motility of Dr. Sutherland’s original conception of a primary respiratory mechanism.
Dr. Upledger’s hypothesis is the most current in the field of cranial osteopathy. Dr. Harold Magun (1976) has cited research that points to rhythmic contraction of the oligodendroglial cells of the neuroglia as a possible cause. of motility and/or fluctuation in the cerebrospinal fluid system. Dr. Upledger does not accept the oligodendroglial cell movement theory as a possible explanation for inherent motility.

The Cranial Rhythmic Impulse

The Cranial Rhythmic Impulse (CRI) or cranial motion, inherent in the primary respiratory mechanism, “occurs in man, other primates, canines, felines, and probably all or most other vertebrates.” (Upledger, 1983, p. 6)
This inherent motion is distinct from respiratory movements and cardiovascular activity. Since the craniosacral system is functionally related to the central nervous system, the autonomic nervous system, the endocrine system, and the neuromusculoskeletal system, the functional integrity of the craniosacral rhythmic impulse has a direct influence on the overall efficiency of the other systems. (Upledger, 1983)
The Mechanical Model and the Pressurestat Model serve to illustrate the primary respiratory mechanism. There are two models that illustrate the two-fold nature of craniosacral motion: 1) the structural motion of the mechanical model, and 2) the fluid motion and its effect upon the central nervous. system which is contained within the pressurestat model.

Structural Motion

There are two phases of structural motion in the reciprocal tension membrane system: flexion and extension. The rhythmic activity of flexion and extension appear “at the sacrum as a gentle rocking motion about a transverse axis located approximately one inch anterior to the second sacral segment.” (Upledger, 1983, p.6)
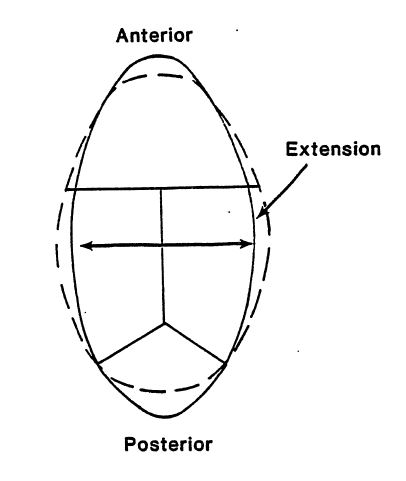
In conjunction with the rocking motion at the sacrum, the transverse dimension of the head will broaden and narrow.
Cyclical flexion and extension occur at approximately six to twelve cycles pe minute; a neutral zone occurs as te bridy passes from flexion into extension. A cycle consists of flexion passing through neutral and entering into extension, thereupon returning to neutral and ending in flexion. One cycle normally takes about six seconds. (Upledger, 1983)
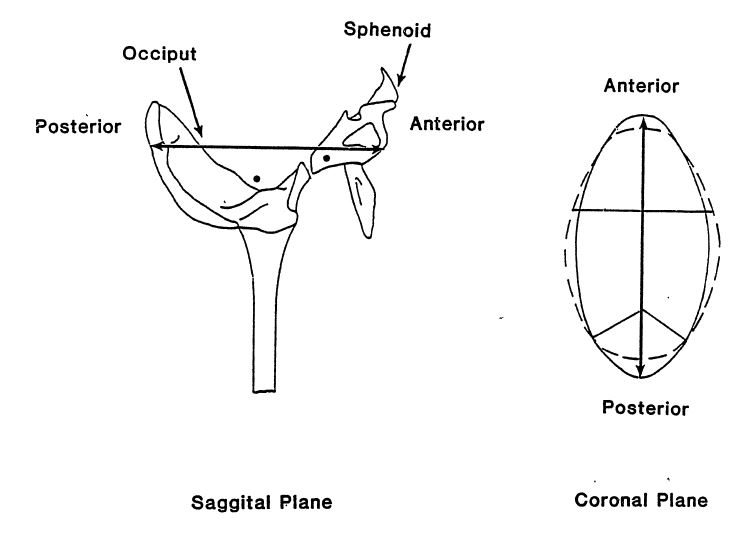
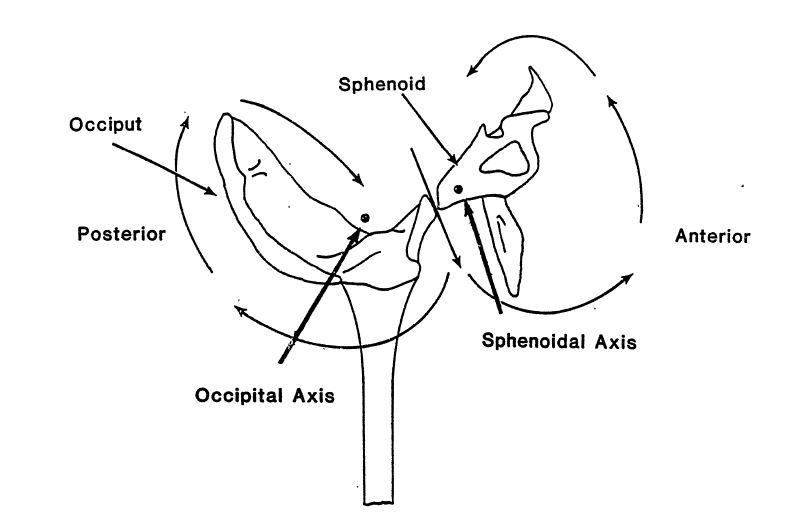
According to Dr. Sutherland’s model, the SPHENOBASlLAR JOINT is the central structure responsible for perpetrating cranial motility. The sphenobasilar joint connects the posterior portion of the sphenoid with the anterior portion of the occiput
(Figure 10) (Upledger, 1983)

This joint is the central part of a larger structure, the CRANIAL BASE. The cranial base includes the sphenoid, the petrous portion of the temporal bones, and the condylar portions of the occiput.
(Figure 11) (Upledger, 1983)

(Figure 11) (Upledger, 1983)

Flexion

During flexion, the entire body broadens and the extremities rotate externally.
There are four key points that clarify the concept of flexion:
1. The transverse dimension of the head widens as a result of the paired bones externally rotating.

(Figure 12A) (Upledger, 1983)
2. The anteroposterior diameter of the skull decreases.

(Figure 12B) (Upledger, 1983)
3. The midline bones of the skull move into FLEXION around a transverse axis located in the sphenoid and the occiput.

(Figure 12C) (Upledger, 1983)
4. The sacral apex moves in an antetoinferior direction and the sacral base moves in a posterior direction away from the symphysis pubis. There is a cephalad pull of the dura due to the elevation of the foramen magnum and the sphenobasilar joint.

(Figure 12D) (Upledger, 1983)

Extension
The movements are the opposite of Flexion
as illustrated in the following diagrams.

1. The transverse dimension of the head narrows and the extremities rotate internally.
(Figure 13A) (Upledger, 1983)
2. The anteroposterior diameter of the skull increases.
(Figure 13B) (Upledger, 1983)
3. The midline bones of the skull move into EXTENSION around a transverse axis located in the sphenoid and the occiput.
(Figure 13C) (Upledger, 1983)
4. The sacral apex moves in an posterosuperior direction and the sacral base moves in anteroinferior direction toward the symphysis pubis. There is a caudal pull of the dura due to the lowering of the foramen magnum
and the sphenobasilar joint.

(Figure 13D) (Upledger, 1983)
Dr. Upledger notes that Dr. Sutherland’s model incorrectly classified the sphenobasilar joint as a symphysis. Histologically, this joint is categorized as a synchondrosis.
This more recent observation by Dr. Upledger is clinically significant. Movements at a synchondrosis are more limited that at a symphysis. (Upledger, 1983) Dr. Sutherland emphasized the osseous nature of cranial base dysfunction evident at the sphenobasilar joint. Dr. Upledger proposes that distortions of the cranial base are the result of abnormal soft tissue or dural membrane tensions and/or sutural immobility rather than a dysfunction of the sphenobasilar Joint itself. (Upledger, 1983) Thus, motion or lack of motion at the sphenobasilar synchondrosis is a manifestation of other restriction(s).
It becomes evident that craniosacral motion involves a flexion and an extension of the dural membrane found in the cranium and in the sacrum. The sphenobasilar joint is a central junction in the osseous structure and the straight sinus is a central junction in the membranous structure. The motion of the osseous and membranous structures is reflected in the positioning of the sacral base and sacral apex; and, this sacral positioning is similarly reflected in the motion of the osseous and membranous structures in the cranium. This totality of motion is made possible through dural tube continuity.

Fluid Motion
“All life is manifested in energy or motion.”
Magoun, 1951, p. 15

The fluid motion of the brain and the central nervous system is graphically illustrated by Sutherland’s analogy with a bird in flight. The central canal of the spinal cord and the fourth ventricle resemble the tail of the bird. The lateral ventricles resemble the wings. As the bird flies, the wings move in and out, anteriorly and posteriorly.
During inhalation, the third ventricle dilates in a V-shaped manner and the floor of the ventricle moves upward. Attached to the floor of the third ventricle is the infundibulum which connects to the pituitary body in the sella turcica. The infundibulum draws the pituitary body upward at the posterior end of the sphenoid while the anterior portion of the sphenoid moves downward. The cerebrospinal fluid fluctuates through the ventricular system during inhalation causing a dilation or expansion of the ventricles.
During exhalation, the ventricles contract and the fluid fluctuates in the opposite direction. This contraction is analogous to the folding of the bird’s wings. (Sutherland, 1967) As the ventricles increase in size during inhalation (flexion), there is a simultaneous increase in the subarachnoid space. The capacity for a greater volume of cerebrospinal fluid is thus increased. The choroid plexuses open out as the ventricles expand and the production of cerebrospinal fluid is increased. (Upledger, 1983)
The osseous nature of the sphenobasilar jolnt emphasized by Dr. Sutherland is thus contained within a fluid motion of the primary respiratory mechanism. According to Dr. Upledger’s hypothesis, the sphenobasilar joint is an integral part of that fluid motion but not the primary cause.
Dr. Magoun (1976) points out that Sutherland’s conclusions were based on the “cerebrospinal fluid physiology in its own natural environment.” (p. 25)
This fluctuation of the cerebrospinal fluid has a physical potency acting as a hydrodynamic mechanism and an electrical potential with positive and negative phases. The electrical potential is directly related to tissue chemistry. The osteopathic approach to disease acknowledges this primary importance of the physical and chemical integrity of body tissues. (Magoun, 1976)
The decade since the publication of Magoun’s third edition of Osteopathy in the Cranial Field has been one of unparalleled discovery in the interdependence of chemical and electrical properties of the brain. R.T. Lustwig wrote:
‘”Sutherland’s work … puts him on record as having recognized at an early date
the interchangeability of energy as it relates to biology … “‘
Magoun, 1976, p. 26

Fascial Continuity
“All life is manifested in energy or motion.”
Magoun, 1951, p. 15

Dr. Upledger emphasizes a concept that is helpful in understanding the comprehensive nature of craniosacral application – fascial continuity. Fascia is a connective tissue composed primarily of, collagenous and elastic fibers. Dr. Upledger proposes and elastocollagenous complex to serve as the contractile mechanism of fascial tissue.
In this model, the elastic fibers are the core. The fascial tissue is regarded as the unifying structure of the body. Fascia is continuous from head to toe. Viscera, muscles, and skeletal structures are present among this continuous network. The central nervous system and the yertebral column are viewed as tubes within this continuous structure.
Fascia is mobile. Dysfunction or injury reduces this fascia} mobility which is then manifested as an abnormal alteration in the physiological motion of the craniosacral system. (Upledger, 1983)
“One may regard the fascial organ as a maze which allows travel from any one place in the body
to any other place without ever leaving fascia.”
(Upledger, 1983, p. 239)
This simplistic reduction of a complex system allows one to comprehend the totality of craniosacral application to the body as a unified whole continuous structure.